Advanced Imaging and AI in Leukemia Diagnosis: Enhancing Accuracy and Care
In the rapidly evolving field of medical diagnostics, advanced imaging techniques are revolutionizing the accuracy and efficiency of leukemia diagnosis, offering hope for better patient outcomes.
The Importance of Early and Accurate Leukemia Diagnosis
Early and accurate diagnosis of leukemia is crucial for effective treatment and improved patient outcomes. Leukemia, a type of cancer that affects blood-forming tissues, can progress rapidly, making timely intervention essential. Detecting the disease at an early stage can significantly increase the chances of successful treatment and long-term remission.
Precision in diagnosis also helps in tailoring treatment plans to individual patients, reducing the risk of complications and improving overall prognosis. Accurate diagnostic techniques can differentiate between various subtypes of leukemia, ensuring that patients receive the most appropriate and targeted therapies.
Leukemia Diagnosis and White Blood Cell Morphology
1. Types of Leukemia
- Acute Lymphoblastic Leukemia (ALL):
- Increased lymphoblasts.
- Blasts often have high nuclear-cytoplasmic ratios, delicate chromatin, and prominent nucleoli.

- Acute Myeloid Leukemia (AML):
- Presence of myeloblasts with azurophilic granules.
- Abnormal forms of myeloid cells can be observed, including promyelocytes and myelocytes.

M2 Acute myeloblastic leukaemia
- Chronic Lymphocytic Leukemia (CLL):
- Small, mature lymphocytes.
- "Smudge cells" (damaged lymphocytes) are often present.

- Chronic Myeloid Leukemia (CML):
- Increased number of granulocytes at various maturation stages (myeloblasts to segmented neutrophils).
- Presence of basophils and sometimes eosinophils.

2. Morphological Features
- Cell Size:
- Blasts are generally larger than normal lymphocytes.
- Nucleus:
- Irregular shapes, increased nucleoli, and clumping of chromatin can indicate malignancy.
- Cytoplasm:
- Myeloblasts may have basophilic cytoplasm and prominent granules.
- Lymphoblasts may have scant cytoplasm.
- Granules:
- Presence of numerous granules in myeloid cells can help distinguish AML.
Acute Myeloid Leukemia (AML)
M0 Acute myeloblastic leukaemia
M1 Acute myeloblastic leukaemia
M2 Acute myeloblastic leukaemia
M3 Acute myeloblastic leukaemia
Microgranular variant of AML-M3
M4 Acute myeloblastic leukaemia
Acute myelomonocytic leukemia (M4) represents 20% of all AML cases. Clinically, 10% of patients exhibit gingival hyperplasia. This leukemia type includes both granulocyte and monocyte components, which vary in proportion and maturation levels. Cytochemically, these cells test positive for chloroacetate esterase, while monocytes show positivity for naphthol-AS-d-acetate esterase or α-naphthyl butyrate esterase.
M4Eo variant: This variant is characterized by at least 5% of cells being abnormal eosinophils, featuring monocytoid nuclei and atypical granules.
M5 Acute myeloblastic leukaemia
M6 Acute myeloblastic leukaemia
M7 Acute myeloblastic leukaemia
Chronic Myeloid Leukemia
Chronic myeloid leukemia (CML) is a type of cancer that affects the blood and bone marrow. It arises from the excessive proliferation of myeloid cells, typically characterized by the Philadelphia chromosome, which results from a translocation between chromosomes 9 and 22, leading to the BCR-ABL fusion gene.
Chronic myeloid leukemia is primarily treated using allogeneic bone marrow transplantation or imatinib (brand name: Gleevec). Allogeneic bone marrow transplantation was once the primary and only treatment option for chronic myeloid leukemia, capable of completely curing the disease. However, with the advent of imatinib (Gleevec), transplantation is now used as a supplementary treatment.
The long-term disease-free survival rate after transplantation is about 60-70%, and it is particularly effective when performed within a year of diagnosis. Imatinib, developed by the Swiss company Novartis, is a groundbreaking treatment for chronic myeloid leukemia, showing excellent results in five-year follow-up studies.
After 18 months of treatment with imatinib, the hematologic complete remission rate reaches an impressive 97%, and the cytogenetic remission rate is 76%. While imatinib treatment cannot completely cure patients, it can safely bring most patients to a state of complete remission, allowing them to lead normal lives. Therefore, it is currently used as the primary treatment for chronic myeloid leukemia.
However, in a small number of patients, imatinib may be ineffective, potentially delaying the timing for allogeneic bone marrow transplantation. Thus, it is crucial to closely monitor the patient's responsiveness to the drug during treatment.
In the 2010s, second-generation targeted therapies such as Tasigna, Sprycel, and Bosulif were developed and marketed. Clinical results have shown these drugs to be significantly superior to the first-generation treatment, Gleevec, in terms of hematologic, cytogenetic, and molecular genetic remission rates, as well as overall survival. Notably, they have proven effective even in patients with intolerance or resistance to Gleevec, transforming chronic myeloid leukemia into a disease managed over a lifetime, similar to hypertension or diabetes.
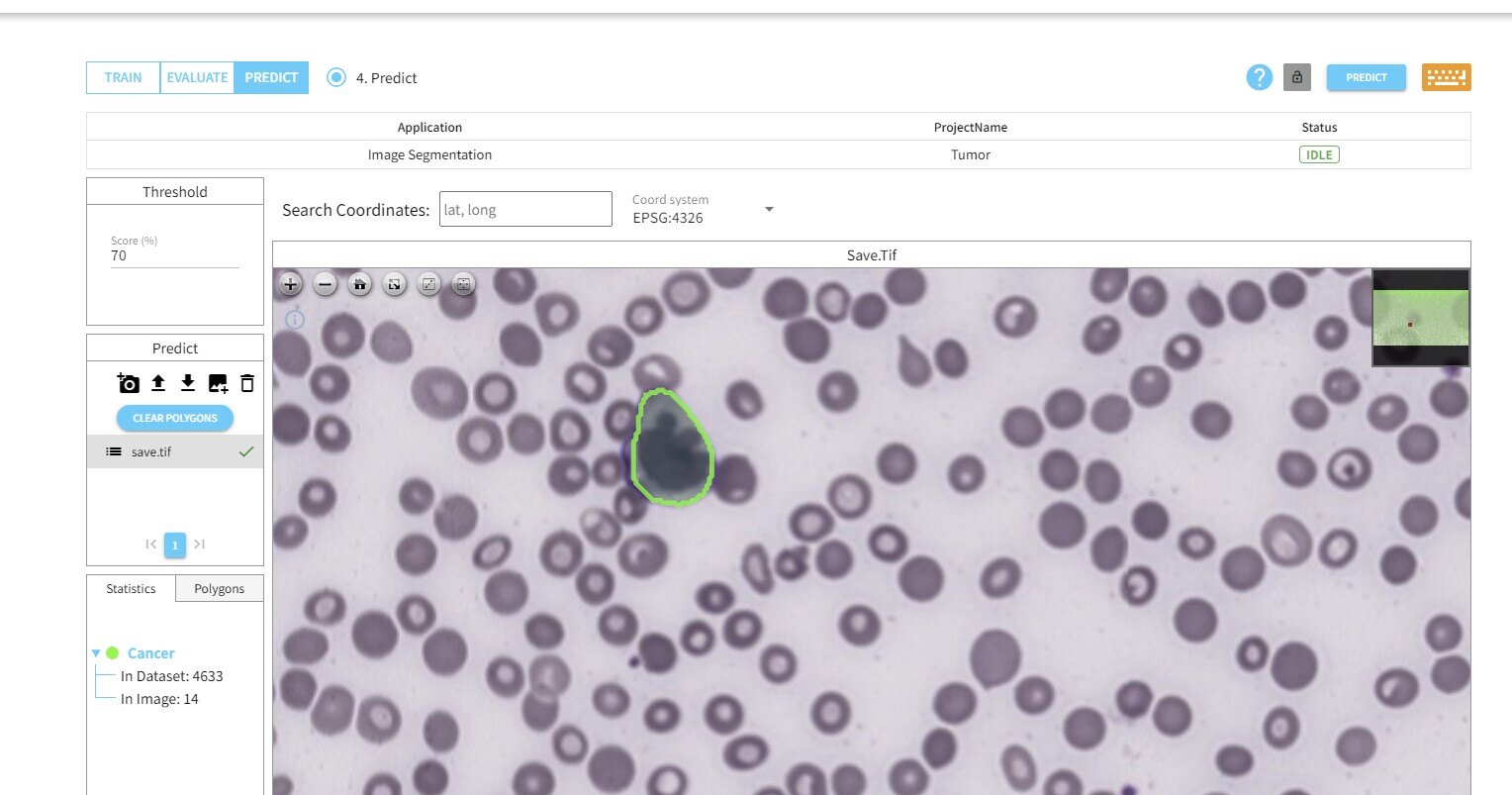
Overcoming Obstacles in Micrograph Analysis Through Automation and deepblock.net
Automation and artificial intelligence (AI) are transforming the field of micrograph analysis. deepblock.net leverage machine learning algorithms to analyze LARGE microscopic images with high accuracy and speed. Users can build their own AI models to identify patterns and anomalies that may be missed by the human eye, reducing diagnostic errors.
By automating the analysis process, deepblock.net and similar platforms enable pathologists to focus on more complex cases and make informed decisions faster. This integration of AI in medical diagnostics not only enhances the accuracy of leukemia diagnosis but also improves overall efficiency, leading to better patient care and outcomes.





