Understanding Albumin and Glycocalyx Health: Insights and Implications
Uncover how albumin interacts with and affects the integrity of the glycocalyx, influencing cellular communication and vascular health.
Exploring the Role of Albumin in Glycocalyx Health
Albumin, a major plasma protein, plays a critical role in maintaining the health of the glycocalyx, the protective layer lining the luminal surface of blood vessels. This protein's interaction with the glycocalyx is pivotal for vascular barrier function and the regulation of tissue fluid balance. Dysregulation in albumin levels can lead to glycocalyx degradation, affecting its permeability and protective functions.
Studies have shown that albumin can bind to components of the glycocalyx, such as glycosaminoglycans, and stabilize its structure. However, when albumin levels are altered, either through disease or injury, this can lead to a compromised glycocalyx and subsequent vascular dysfunction.
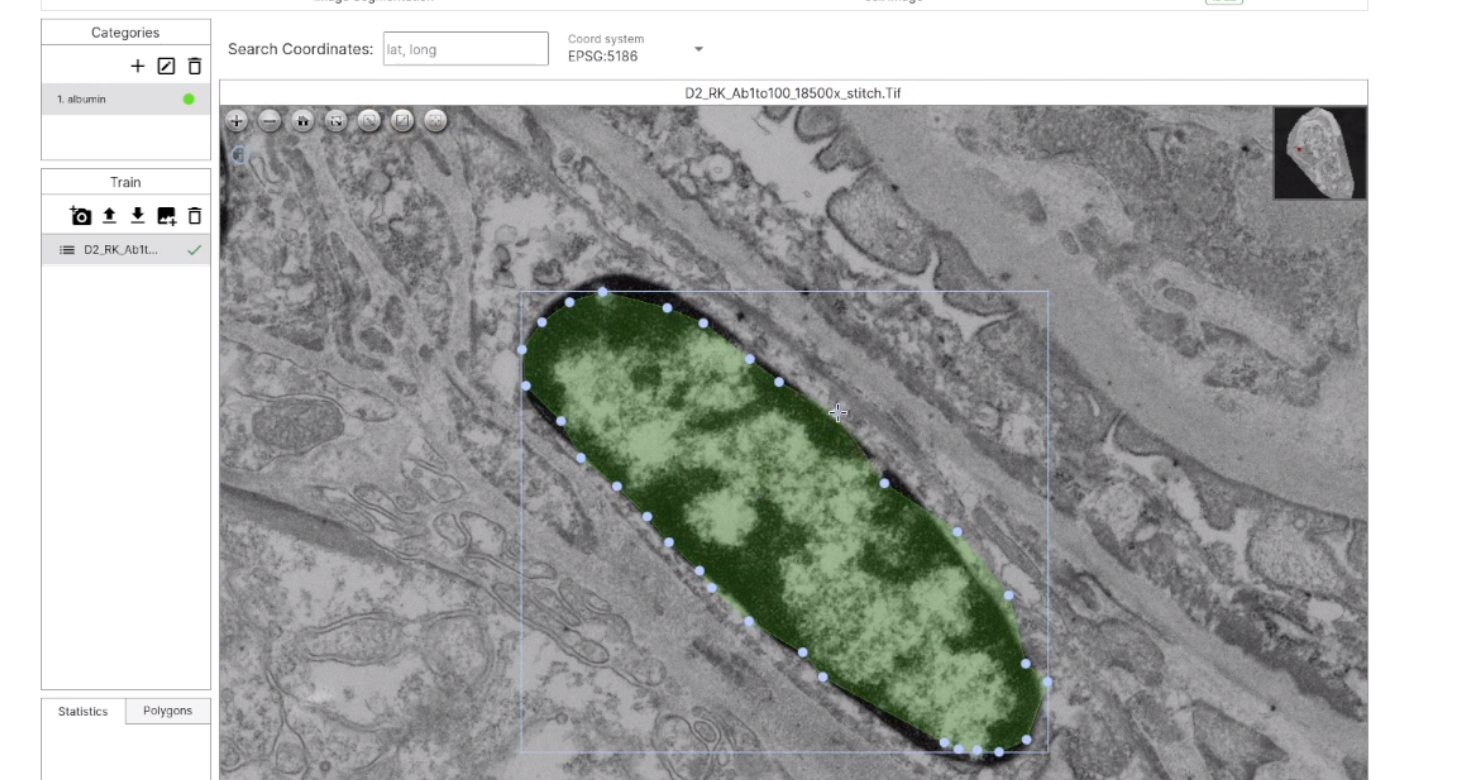
The video showcases the process of utilizing Deep Block technology to create an AI model that identifies and extracts areas where albumin is present within a large TEM micrograph.
Factors Contributing to Proteinuria
Proteinuria, the presence of abnormal levels of protein in the urine, is often a sign of kidney damage. Several factors contribute to its development, including hypertension, diabetes, and genetic predispositions. Albumin, being the main protein in blood plasma, is commonly found in proteinuria, indicating a breakdown in the filtration barrier of the kidneys.
Chronic conditions that affect the integrity of the glomerular basement membrane or the glycocalyx can lead to proteinuria. Additionally, enzymatic actions, such as those by hyaluronidase on the glycocalyx, can degrade this barrier and permit albumin to leak into the urine.
Diabetes-Induced Proteinuria and Its Mechanisms
Diabetes mellitus is a significant risk factor for the development of proteinuria. High blood glucose levels associated with diabetes can induce changes in the kidney's filtration system. These changes include thickening of the basement membrane, loss of podocyte integrity, and degradation of the glycocalyx, all of which contribute to the leakage of albumin into the urine.
The mechanisms behind diabetes-induced proteinuria include the non-enzymatic glycation of proteins and increased oxidative stress, which can damage the glycocalyx and alter its ability to prevent albumin loss.
Diabetes damages the kidneys primarily through a condition known as diabetic nephropathy, which is a progressive kidney disease caused by long-term elevated blood glucose levels. Here’s a detailed explanation of how diabetes affects the kidneys:
Pathophysiology of Diabetic Kidney Damage
-
Hyperglycemia and Glomerular Damage:
- High Blood Sugar Levels: Chronic hyperglycemia (high blood glucose) causes the kidneys to filter more glucose, which can damage the glomeruli (the filtering units of the kidneys).
- Glomerulosclerosis: Elevated glucose levels lead to the accumulation of advanced glycation end-products (AGEs), which can cause inflammation and scarring of the glomeruli. This process, known as glomerulosclerosis, impairs the kidneys' filtering ability.
-
Increased Intracellular Glucose and Metabolic Changes:
- Hyperfiltration: Initially, the kidneys may respond to high blood sugar levels by increasing the filtration rate to cope with the excess glucose. This hyperfiltration puts additional stress on the glomeruli and can eventually lead to kidney damage.
- Glucose Toxicity: High levels of glucose within kidney cells can cause cellular injury and contribute to oxidative stress, further exacerbating kidney damage.
-
Inflammation and Fibrosis:
- Inflammatory Responses: Chronic hyperglycemia triggers inflammatory responses within the kidney tissues. Inflammation contributes to the development of fibrosis (scar tissue formation) in the kidneys.
- Renal Fibrosis: Fibrosis impairs kidney function by replacing healthy kidney tissue with non-functional scar tissue, leading to a progressive decline in kidney function.
-
Hypertension and Renal Damage:
- Diabetic Nephropathy and Blood Pressure: Diabetes often coexists with hypertension (high blood pressure), which further aggravates kidney damage. Elevated blood pressure increases the pressure within the glomeruli, accelerating glomerular injury and protein leakage into the urine.
- Renin-Angiotensin System: Diabetes can activate the renin-angiotensin-aldosterone system (RAAS), leading to further hypertension and kidney damage. RAAS activation contributes to increased blood pressure and worsening of kidney function.
-
Proteinuria:
- Protein Leakage: Damage to the glomeruli increases their permeability, allowing proteins (such as albumin) to leak into the urine. Persistent proteinuria is a key marker of diabetic nephropathy and indicates ongoing kidney damage.
Implications of Glycocalyx Damage in Vascular Diseases
The glycocalyx serves as a crucial barrier and sensor within the vascular system, and its damage can have profound implications for vascular health. Degradation of the glycocalyx has been implicated in the pathogenesis of atherosclerosis, hypertension, and thrombosis. Albumin leakage into the vessel wall due to glycocalyx breakdown can lead to inflammation and plaque formation.
Understanding the interaction between albumin and the glycocalyx is essential for developing therapeutic strategies to prevent and treat vascular diseases. Protecting the glycocalyx may help to maintain vascular homeostasis and prevent the progression of cardiovascular disorders.
Assessing Drug Toxicity and Its Impact on Glycocalyx Health
Drug toxicity can lead to proteinuria, which is the presence of excess protein in the urine. This relationship is particularly important because proteinuria can be a marker of kidney damage, which may be caused by the toxic effects of certain medications. Here’s a detailed look at how drug toxicity relates to proteinuria:
Direct Nephrotoxicity:
- Some drugs have direct toxic effects on kidney cells, including the glomeruli (the filtering units of the kidneys). This damage can increase the permeability of the glomerular filtration barrier, allowing proteins (like albumin) to leak into the urine.
- Examples include certain antibiotics (e.g., aminoglycosides), nonsteroidal anti-inflammatory drugs (NSAIDs), and some chemotherapeutic agents.
Immunological Reactions:
- Certain drugs can induce allergic or immunological reactions that affect the kidneys. Conditions like drug-induced lupus nephritis or glomerulonephritis can lead to proteinuria.
Altered Renal Hemodynamics:
- Some medications affect renal blood flow or blood pressure, which can alter the kidney’s ability to filter blood properly. For instance, drugs that impact the renin-angiotensin system (like ACE inhibitors or angiotensin receptor blockers) can sometimes cause changes in kidney function that lead to proteinuria.
Toxic Metabolites:
- Drugs that are metabolized into toxic metabolites can affect kidney function. For instance, drugs like cisplatin (a chemotherapeutic agent) can generate nephrotoxic metabolites that damage renal cells and lead to proteinuria.